LET ME SHOW YOU THE DATA
Why dieting doesn't usually work | Sandra Aamodt
- YouTube
How to get healthy without dieting | Darya Rose | TEDxSalem
- Bing video
- HAES_publicationAJPH.2013.301486.pdf
- Benefits of weight inclusive approach
- Weight Science: Evaluating the Evidence for a Paradigm Shift | Nutrition Journal | Full Text (biomedcentral.com)
- Homepage | Weight Neutral For Diabetes Care (wn4dc.com)
- ASDAH | Committed to Size Diversity in Health and HAES®
- Academy of pediatrics no weight loss peds.2016-1649.full.pdf
Myth/claim/assumption: Increased weight causes decreased health and weight loss cures any illness caused by increased weight.
What research shows: Weight may be related/linked/associated to illnesses such as hypertension, diabetes and hyperlipidemia, but there is no evidence of a causal effect. Many genes have been identified that cause both insulin resistance/increased weight and health issues. Healthy behaviors can affect insulin resistance to some degree, but studies show it has just 5-7% decrease in weight. In reality when weight loss is examined separately from healthy behavior, weight loss itself has a negative effect on health/death rate regardless of if weight loss was intended or not. With healthy behavior, health benefits can result with or without weight loss.
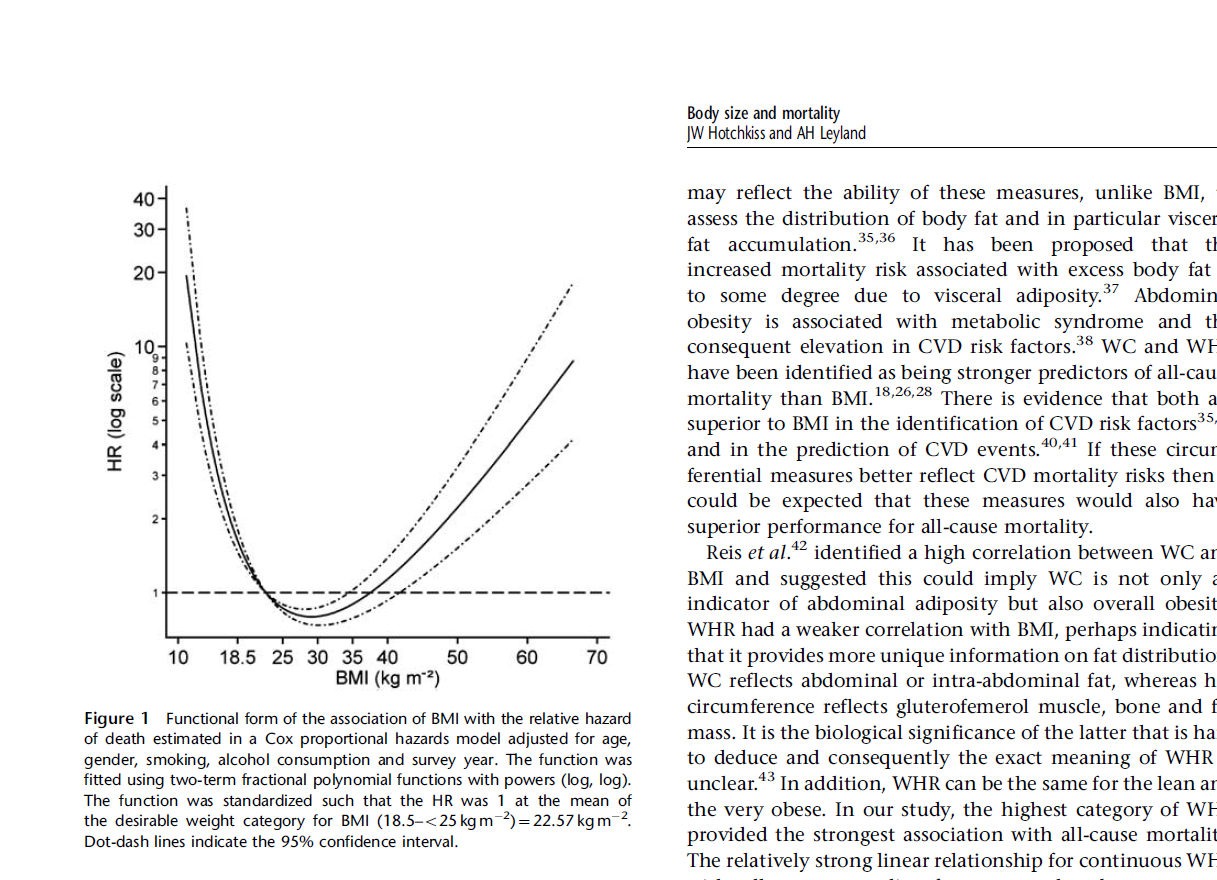
In actuality, we have a lot of data (known as “The Obesity Paradox”) that shows that those in the “overweight” and “obesity” category actually in reality on average live longer than those in the “normal” weight category. Those in the underweight category have worse outcomes than even the “morbid obese” category. This obesity paradox is true in patients with diabetes, heart disease, renal failure, cancer, congestive heart failure among many others.
higher BMI not a risk for orthopedic surgery.pdf
Carnethon_meta-anal_obesity_paradox_in_diabetes.pdf
Doehner_et_al_2012_weight_loss_makes_it_worse.pdf
Fitness_vs_fatness_in_Proceedings_in_Cardiovas.pdf
Fitness-Fatness___survival_in_those_with_predi.pdf
Obesity_paradox_in_Heart_failure-proceedi-0001.pdf
Obesity_paradox_in_Kidney_disease-Proceedings_.pdf
Myth/claim/assumption: Obesity is growing at an alarming rate
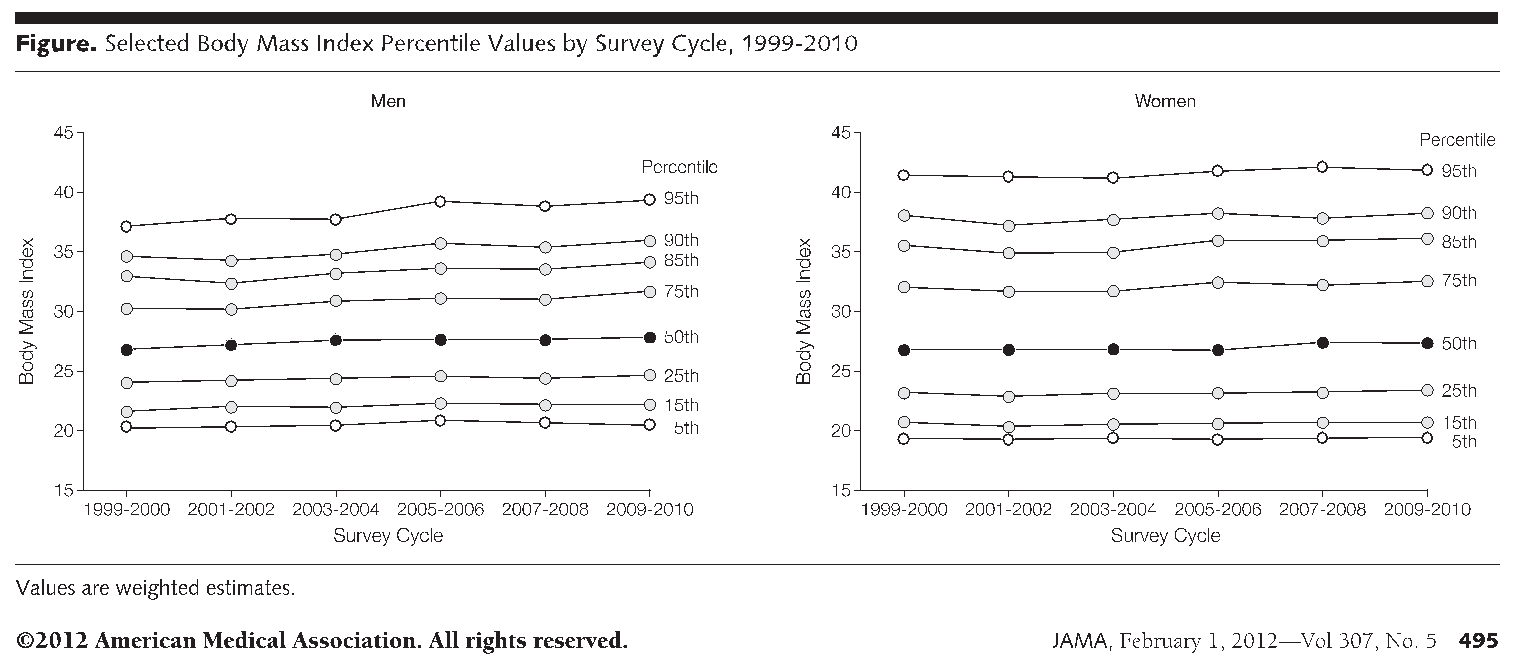
What research shows: The very commonly used slides from the CDC that show drastically increasing weights are based on research done by non-randomized phone calls (not a single person weighed or measured.) Research done by actually weighing and measuring people over time (such as NHANES data) do not show such drastic changes in weight and are actually leveling off or decreasing. Also, some of the change in percentages of people considered to be “overweight” or “obese” is due to changes in criteria made in 1998. Also things such increased use of pesticides, herbicides, increase in air pollution, use of preservatives have had an effect on our environment as well (so it is not simply behavioral changes.)
Myth/claim/assumption: Weight loss is a simple equation of eating less and exercising more and anyone can do it if they follow instructions and have enough “will power.” All we need to do as healthcare providers is explain to people how important it is to lose weight. If people do not lose weight, they are doing something wrong.
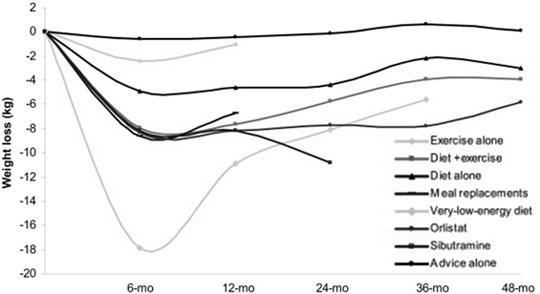
What research shows: Fewer than 5% of people who attempt weight loss can lose more than about 20 pounds and keep it off (even when they do healthy behavior consistently.) This often leads weight cycling or yo-yoing (weight going up and down) which research undeniably shows is worse than being large. 1/3 to 2/3 of participants end up weighing more than when they started the program.
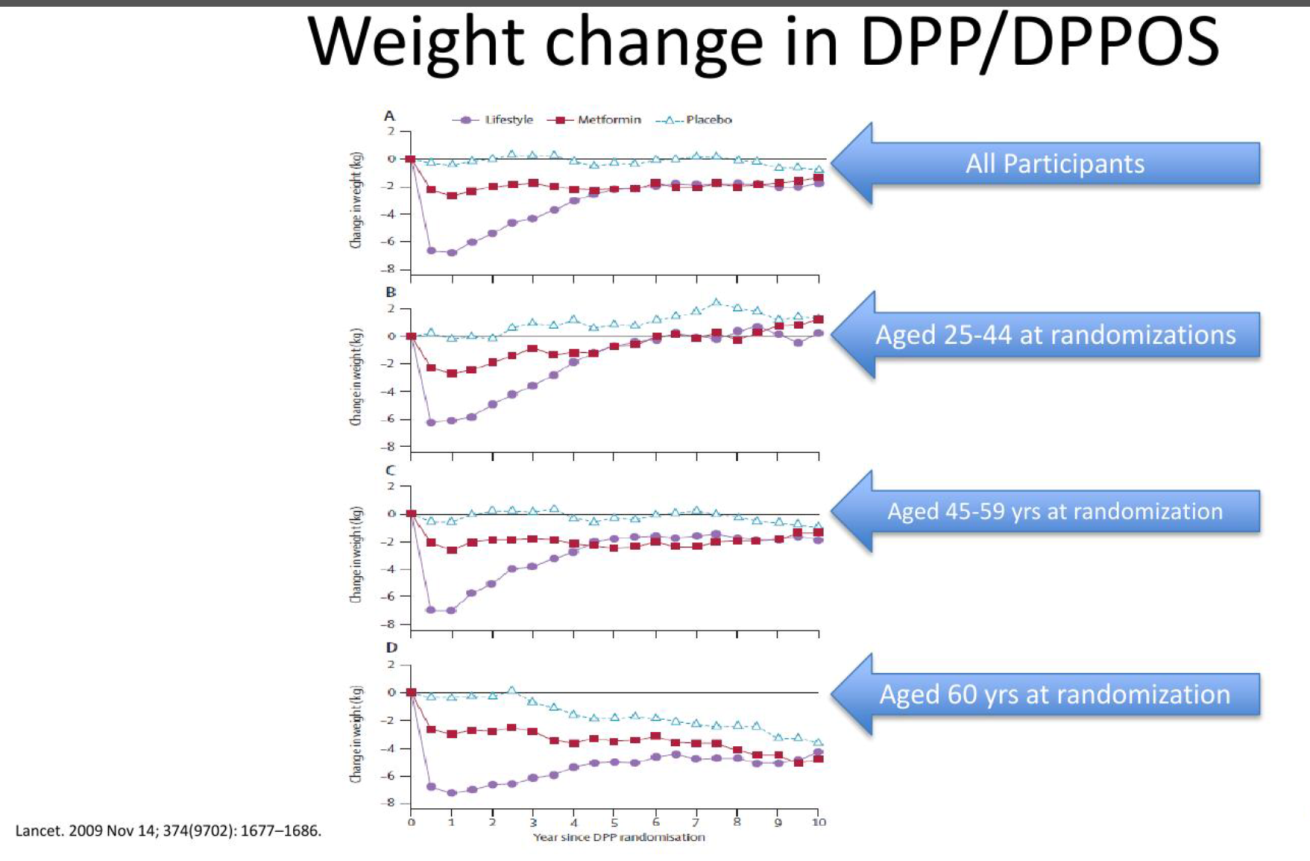
This is true for even large labor-intensive studies such as “The Diabetes Prevention Trial” or “The Look Ahead Trial.” The “Diabetes Prevention Trial” was a 4-year study that was extended to a 10-year study encouraging healthy behavior to “prevent” diabetes. Initially there was a 5-7% weight loss but at 10 years the difference was only slight. The Look Ahead Trial was a 10-year multicenter, randomized clinical prospective study with over 5000 participants (very well-designed study.) This study was designed to show that weight loss would benefit health. Quite to the contrary at the end of 10 years, weight loss efforts did not decrease incidence of diabetes or change death rate. Rather than report that weight loss efforts did not decrease health risk, they reported “people can lose weight and keep it off.” In reality the difference in weight loss at 8 years was 2.1% difference (less than 5 pounds for a 200-pound person.) There are a lot of large people who consistently do healthy behavior (that we think should cause weight loss) and a lot of thin people who do not do as much healthy behavior.
We have identified over 100 genes related to weight/insulin resistance.
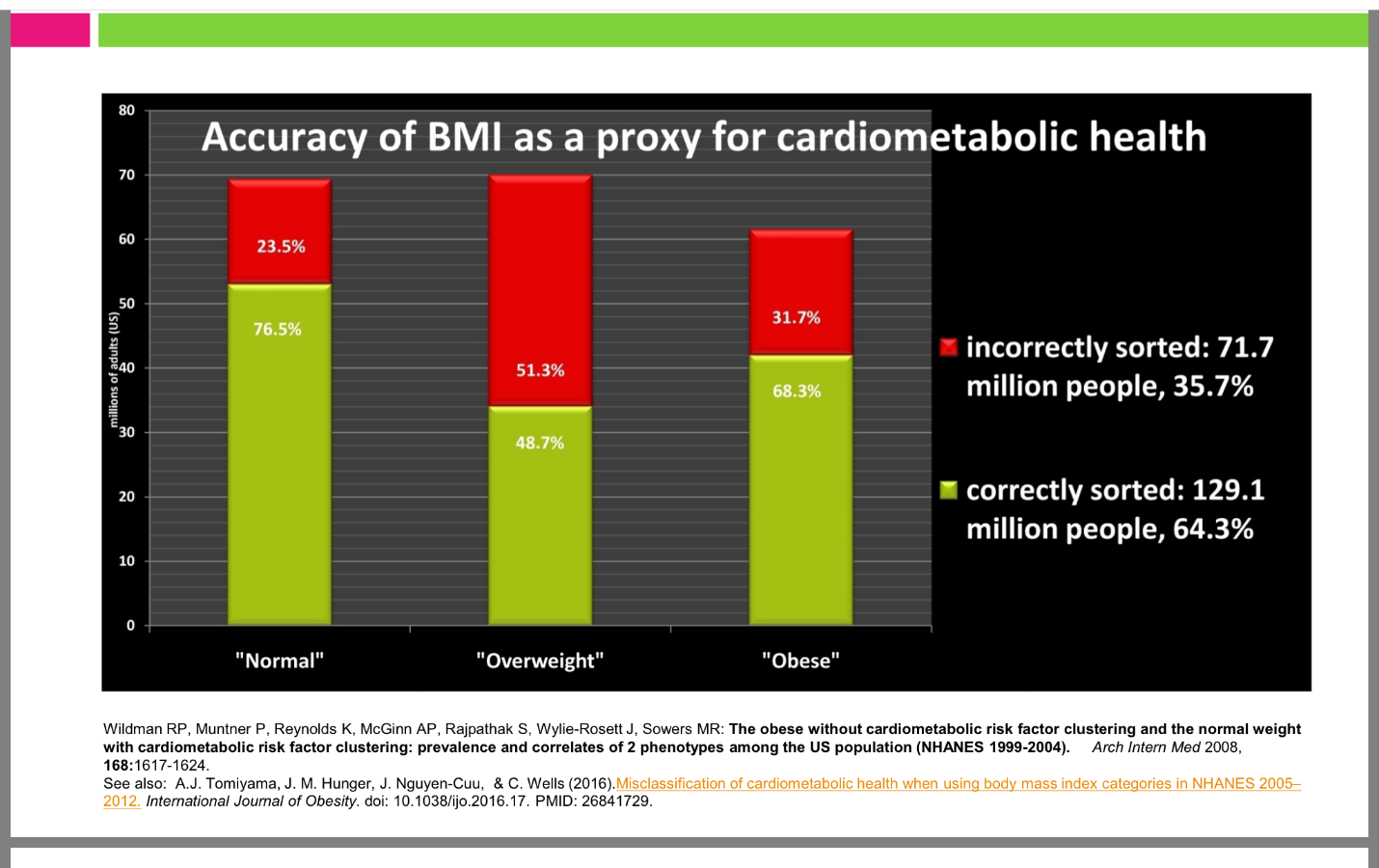
Myth/claim/assumption: BMI is an accurate predictor of health
What research shows: 23.5% of people in a “normal” BMI category have poor cardiometabolic health and the opportunity to help them improve health with healthy behavior will be lost if it is assumed that they are cardiometabolically healthy simply because they have a “normal” BMI. 31.7% of those in an “obese” category are cardiometabolically healthy. Thin people who are insulin resistant have much worse health outcomes than larger people even if larger people are insulin resistant. Thin people with diabetes have worse health outcomes than larger people with diabetes.
Myth/claim/assumption: Encouraging weight loss is helpful
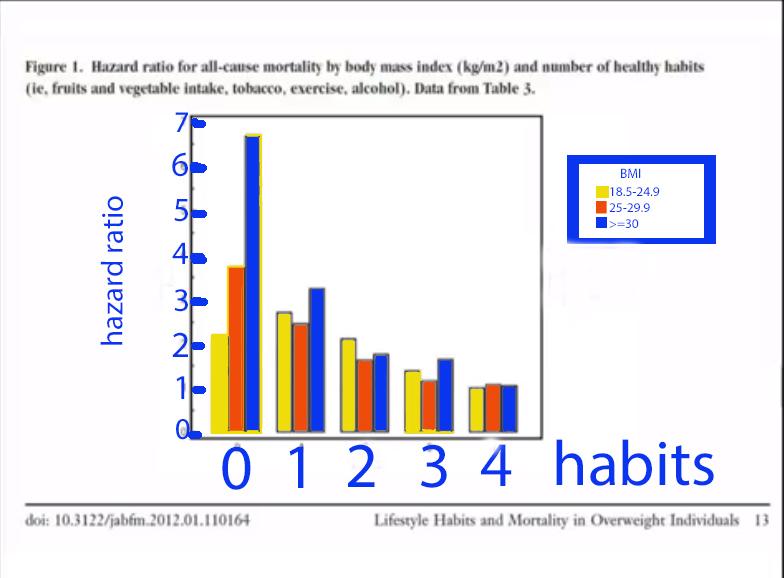
What research shows: Telling someone with excess weight that weight loss can be achieved by simple behavior change is the same as telling them that their weight is their fault. Placing blame leads to stigma which decreases health and leads to a lot of discrimination. Studies actually show that even those who are in a “normal” weight category are harmed by weight loss efforts. Even telling someone to lose 5-7% of excess weight leads to stigma, as you cannot tell by assessing BMI, weight, or waist circumference how much healthy behavior someone is already doing. If they are already doing healthy behavior, it is unlikely that they will be able to lose and sustain even a 5-7% weight loss. This can lead to feelings of failure even if they are doing a lot of healthy behavior. We could help people be healthier if we focus on fitness for ALL people (including those who have a “normal” BMI) rather than weight loss. Fitness makes much more difference than fatness/BMI in mortality and health issues. Weight loss without healthy behavior such as with liposuction does not benefit health. Even if weight loss remains the goal, the behavioral goals need to be for behaviors and weight loss is not a behavior! Finding a positive behavior and focusing on it/reinforcing it rather than placing blame and shame on negative behavior has been well established as more successful.
Myth/claim/assumption: All research is unbiased and all research findings are published and accessible. Advertisements promising weight loss are true and accurate.
What research shows: Weight loss research is often funded by the 60 billion dollar a year weight loss industry. Even non-profit organizations such as the American Diabetes Association and Academy of Nutrition and Dietetics are supported by industry. Weight loss is often sensationalized by celebrities who claim to be “experts.” Weight stigma is strong in the medical profession and national organizations such as the CDC. After publishing very strong data showing the “Obesity Paradox” Katherine Flegal published a statement on the horrendous treatment/treats she faced from her colleagues for 10 years. The American Diabetes Association published that Flegal’s research had been debunked by Tobias study published in NEJM 2014; 370:233-244. In order to achieve only slightly statistically significant data showing a linear relationship between weight and health, Tobias had to significantly manipulate the data to make the j-curve linear. The fact that a peer reviewed journal published this significantly manipulated data and the most respected non-profit organization in diabetes care acknowledged that this debunks much more justified data shows how much weight based discrimination there is in the health care system. In the Tobias study they:
1. Eliminated underweight category entirely
2. Used only upper end of normal as reference. If they would have used the whole normal range, the j-curve would have remained.
3. Had to eliminate those over 65
4. Had to eliminate those that never smoked
5. Does not mention, that even if it is linear, you have to compare the upper end of normal to obese class 1 to get slight statistical significance and even obese class II and III is not compelling evidence of a relationship. May not even be significant at all even comparing normal to obese class II-III if whole normal weight category used as reference
6. Still does not show causality or that weight loss helps
Let me “show you” the data:
Myth/claim/assumption: Conclusions on research studies always report accurately
What the research shows: Often conclusions are not always accurately or completely stated. For example, the conclusion of the famous “Diabetes Prevention Trial” was that “Diabetes can be prevented 58% of the time with weight loss.” This is the study that is often referred to when it is stated weight loss “prevents” diabetes. In reality what this study showed is that diabetes can be delayed 58% of the time with healthy behavior at 4 years. By 10 years this was decreased to 34% difference. Important to note is that despite very labor-intensive efforts to maintain weight loss, there was very little difference in weight by the end of 10 years between the study group and the control group. This is more indicative that the difference in health benefit was more due to healthy behavior than the weight loss itself (The Diabetes Prevention study did not differentiate the benefit of weight loss from the benefit of healthy behavior.) Studies that did differentiate between the benefit of fitness and weight loss itself, support that the benefit is more related to changes in behavior rather than the weight loss itself.
Myth/claim/assumption: Weight loss surgery “cures” diabetes
What the research shows: A decrease in calories improves insulin sensitivity and decreases the need for insulin. Diabetes is simply an equation between the amount of insulin needed vs the amount of insulin that can be produced. If that gap is small, a decrease in the amount of insulin needed can close that gap and make it so that medication is no longer needed to control the blood sugar (claimed as a “cure”.) However, if that gap is larger, the decrease may not be enough to close the gap and despite the decrease in calories after the surgery, they will continue to need medications to control the blood sugar. As we age, we need more insulin and can produce less. So as time goes on the gap can increase again, so even if medication is no longer needed to control blood sugar, it is often short lived. Some say that weight loss surgery itself changes gut hormone secretion and this is what leads to the “cure” of diabetes. The attached article shows that you can get the exact same hormone changes in severe calorie reduction with or without surgery. Meaning that the changes in hormone production are likely more due to the calorie restriction after weight loss surgery rather than the surgery itself. They also claim that because the “cure” occurs before weight loss that it was the surgery that cured the diabetes not the weight loss. In reality, it is the decrease in calories not the weight loss or the surgery that decreases the need for insulin.